Cranial Dystonia, Blepharospasm and Hemifacial Spasm:
Clinical Features and Treatment, Including the use of Botulinum Toxin
Stephen P. Kraft MD, FRCSC,
Department of Ophthalmology, University of Toronto;
Anthony E. Lang MD, FRCPC,
Movement Disorder Clinic, Toronto Western Hospital
Contents:
- Clinical Features and Course
- Cranial dystonia
- Blepharospasm
- Additional Abnormal Movements
- Hemifacial spasm
- Epidemiologic Features
- Cranial dystonia
- Hemifacial spasm
- Pathophysiologic Features
- Cranial dystonia
- Hemifacial spasm
- Differential Diagnosis
- Cranial dystonia
- Hemifacial spasm
- Table 1
- Disorders considered in the differential diagnosis of blepharospasm
- Treatment
- Cranial dystonia
- Medical
- Surgical
- Hemifacial spasm
- Medical
- Surgical
- Botulinum toxin injections
- Pharmacologic features
- Method of treatment
- Results of treatment
Clinical Features and Course
Blepharospasm, the most frequent feature of cranial dystonia, and hemifacial spasm are two involuntary movement disorders that affect facial muscles. The cause of blepharospasm and other forms of cranial dystonia is not known. Hemifacial spasm is usually due to compression of the seventh cranial nerve at its exit from the brain stem. Cranial dystonia may result in severe disability. Hemifacial spasm tends to be much less disabling but may cause considerable distress and embarrassment. Patients affected with these disorders are often mistakenly considered to have psychiatric problems. Although the two disorders are quite distinct pathophysiologically, therapy with botulinum toxin has proven very effective in both. We review the clinical features, proposed pathophysiologic features, differential diagnosis and treatment, including the use of botulinum toxin, of cranial dystonia and hemifacial spasm.
Dystonia is defined by a subcommittee of the Dystonia Medical Research Foundation as a syndrome dominated by sustained muscle contractions, frequently causing twisting and repetitive movements or abnormal postures (unpublished definition). The involuntary movements can vary from brief spasm to sustained contractions. In cranial dystonia the involuntary spasms are bilateral and involve eyelid, facial, mandibular, oral, lingual and laryngeal muscles. [1] Synonymous terms for this entity include Meige's syndrome, Breughel's syndrome, idiopathic orofacial dystonia, blepharospasm-oromandibular dystonia and cranial-cervical dystonia. Its most frequent presenting sign is blepharospasm.[2-4]
Unilateral spasms of the eyelid and perioral muscles innervated by the facial (seventh cranial) nerve is a disorder known as hemifacial spasm. [5,6] It is not considered a form of cranial dystonia. However, the two disorders have overlapping clinical features, and both respond to therapy with botulinum A exotoxin.
Frequently patients with these disorders are mistakenly considered to have psychologic problems. Thus, many affected people, some of whom may be functionally blind, are not properly referred for neurologic assessment and treatment.
Cranial Dystonia
Most cases of cranial dystonia develop and progress slowly over a number of years. Rarely the onset is sudden. [3] Symptoms may stabilize in mild cases. Some patients have a fluctuating course, with exacerbations and partial remissions.[4] About 1% of patients have spontaneous total remission.[4]
» Blepharospasm
Blepharospasm is the most frequent feature of cranial dystonia.[2-4] If the dystonia is limited to the eyelids it is termed "essential blepharospasm". [3] Intermittent or persistent contractions of the orbicularis oculi muscles cause the eyelids to clamp tightly shut. In most patients blepharospasm is preceded by an increase in the frequency of blinking. Other early complaints include dry eye symptoms (foreign-body sensations, grittiness and eye irritation) and photophobia (extreme sensitivity to bright light). [3] In approximately 25% of patients the symptoms begin in one eye, but they become bilateral in almost all cases. However, the degree of involvement may remain asymmetric. [4]
Once the orbicularis oculi contractions are well established they may be tonic and sustained, brief and clonic, or regular and rhythmic. Patients frequently complain of retro-orbital discomfort at the time of the spasms. In many cases there are precipitating factors, such as bright light, driving, chewing, stress, emotion and anxiety-provoking social situations. [3,4] There is often relief for the first 1 or 2 hours after awakening in the morning. Patients may adopt sensory "tricks", such as yawning, extending the neck, singing, whistling and wearing dark glasses, to reduce or hide the manifesting symptoms. [3] Patients with severe spasms have to manually pry their eyes open and keep pressure on the upper eyelids to prevent the spontaneous closure.
Increased attention or concentration, such as occurs in the physician's office, can temporarily reduce the severity of blepharospasm, even in a severely affected patient. Consequently, the severity can be grossly underestimated if one relies solely on the amount of disability seen during an interview. The variability in severity of symptoms, the unusual aggravating and relieving factors, and the discrepancy' between the history of the disorder and objective signs seen by the physician have often resulted in the condition's being misdiagnosed as hysteria or other psychiatric disorders. [3]
Patients who are severely affected may be rendered functionally blind for substantial periods of the day. Sudden involuntary lid closure can occur while a patient is driving or crossing the street and thus can result in injury. Many such patients become social recluses.
» Additional Abnormal Movements
Blepharospasm associated with dystonic movements of other muscle groups in the face, neck or limbs is known as Meige's syndrome. Involvement of lower cranial muscles is seen in a large number of such patients and is referred to as oromandibular dystonia.[2,3] Abnormal movements include retraction and forced opening of the mouth, tensing of the platysma, jaw clenching, pursing and tightening of the lips, flaring of the nostrils, dystonia of the tongue (including involuntary protrusion) and contractions of the soft palate and floor of the mouth.
The earliest symptom is usually "action dystonia" - that is, the involuntary movements appear only when the involved muscles are used (such as in talking or chewing). Typically one action may precipitate the dystonia; other actions may, at the outset, not be involved at all.[4] As the disorder worsens, more and more actions are affected, and the spasms become more intense. Eating, swallowing and speech all may become impaired. Forced jaw closure may damage the lips, gums and tongue. Teeth may be cracked, and it may be impossible to maintain dentures in place. Temporomandibular joint pain may occur, along with recurrent jaw dislocation.
Other muscle groups that may also be affected by dystonic movements include muscles of the pharynx[7] and larynx.[3,8] The voice may become harsh, hoarse and strained, a condition termed spasmodic dysphonia.[8] Cervical muscle involvement, typical of spasmodic torticollis, may accompany cranial dystonia; less often distal muscles, such as of the hand (as in "writer's cramp"), may be affected. A postural tremor similar to benign essential tremor often accompanies cranial dystonia, and occasionally parkinsonian symptoms are present (not to be confused with cranial dystonia as a complication of levodopa therapy).[9,10]
Hemifacial spasm
In contrast to blepharospasm and other features of cranial dystonia, hemifacial spasm is unilateral. Rarely the disorder is bilateral; in such cases the movements on the two sides of the face are asynchronous, in contrast to the simultaneous bilateral movements of cranial dystonia.
In the typical form of the disease the continuous unilateral facial muscle twitching first affects the orbicularis oculi. The paranasal and perioral muscles and platysma subsequently become affected in almost all patients.[5] The twitches, which are usually clonic, are mild at the onset. They may become tonic as the disease worsens and cause persistent closure of the eye and tensing of other affected muscles.[5,6] Voluntary activation of one area (e.g., the frontalis, by asking the patient to elevate the brow) frequently causes contraction of other facial muscle groups and often provokes the involuntary spasms.
A small proportion of cases of hemifacial spasm represent a postparalytic form that develops as a sequela of facial nerve palsy (Bell's palsy) or injury. In addition to the clonic twitches there are often synkinetic movements among several facial muscles on the affected side. In this form of hemifacial spasm there is residual facial weakness on the affected side, whereas in the typical form the facial weakness is more apparent than real.[6,11]
In contrast to cranial dystonia, the spasms in hemifacial spasm may persist during sleep, and the movements, in general, cannot be altered by sensory tricks. However, emotion and stress frequently aggravate the condition.[5,6]
Epidemiologic Features
» Cranial Dystonia
Idiopathic cranial dystonia has its peak onset in the sixth decade of life.[2,3] Women are affected more frequently than men, the female:male ratio ranging from 3:2 to 2:1.[2,3,12] The prevalence rate of cranial dystonia is estimated at 5 to 10 per 100 000 population.[13]
The disorder is usually sporadic, but there are a few reports of familial occurrence, some of which suggest an autosomal dominant pattern with incomplete penetrance.[3,14,15] Various medical problems, including depression,[2,3,16] thyroid disease[3,17,18] and autoimmune disorders,[3] are frequently reported in patients with cranial dystonia. Some investigators have found a high incidence of other neurologic disorders in families of patients with cranial dystonia, the most frequent being essential tremor and Parkinson's disease.[3] However, other than an affiliation with depression and a higher than normal incidence of familial tremor, we have not been able to confirm these associations (unpublished observations).
» Hemifacial spasm
The typical form of this disorder has an insidious or subacute onset in the third to the seventh decade, with a peak in middle age. It is more frequent in women.[5,19] The common form (i.e., not a sequela of Bell's palsy) is caused by lesions affecting the root of the facial nerve. There is no predilection for right- or left-sided involvement.[5,6] The disorder usually occurs in isolation; however, occasionally it is associated with trigeminal neuralgia[5] or other concomitant cranial nerve dysfunction.
Pathophysiologic Features
» Cranial dystonia
The precise cause of cranial dystonia is not known. Similar movements may be caused by levodopa therapy in Parkinson's disease and by dopamine receptor antagonists (e.g., neuroleptic antipsychotic drugs and metoclopramide hydrochloride), both suddenly (acute dystonic reactions) and after long-term therapy (tardive dystonia). This suggests that the neurotransmitter dopamine may play an important role in the development of the abnormal movements.
A small number of patients with lesions in the rostral midbrain or caudal diencephalon were reported to have abnormal movements similar to those in cranial dystonia.[20-22] Jankovic and Patel[20] suggested that the abnormality may have been due to supranuclear disinhibition of the facial nucleus and brain-stem reflexes, denervation supersensitivity of the facial nuclear complex, sprouting of surviving axons or some combination of the three. No consistent pathological features in the brain stem or basal ganglia have been found in postmortem specimens.
Recently postmortem biochemical studies of a single case without histologic abnormalities showed the dopamine levels to be three times higher than normal in the red nucleus.[23] In addition, the norepinephrine levels were two times higher than normal in the red nucleus and four times higher in the substantia nigra; there were also changes in the levels of norepinephrine's chief metabolite in the internal globus pallidus. Positron emission tomography (courtesy of Dr. E. Stephen Garnett, McMaster University, Hamilton, Ont.) in one of our patients, an 81-year-old woman with cranial dystonia and writer's cramp, showed a decrease in dopamine activity in the left putamen, whereas levels in the right putamen were within normal limits.
Electrophysiologic studies have shown increases in the amplitude and duration of the Rland R2 components of the blink reflex and corneal reflex, with normal latency values.[24,25] After a conditioning shock the recovery of the R2 component of the blink reflex is abnormally rapid. These results suggest that an abnormal excitatory drive to facial motor neurons and interneurons may be mediating these reflexes.[24]
The pharmacologic basis of cranial dystonia is controversial. There have been reports of dopaminergic preponderance,[26] dopamine receptor hypersensitivity[27] and excessive activity in both dopaminergic and cholinergic systems.[28] However, the response of cranial dystonia to medical therapy has been unpredictable and inconsistent from patient to patient. The disease may be a heterogeneous disorder with more than one pharmacologic subtype.
» Hemifacial spasm
The typical form of hemifacial spasm is caused by compression of the facial nerve at its exit from the brain stem or, less commonly, at its entry into the internal auditory meatus.[5,19,29,30] The most frequent finding at the time of neurosurgical exploration is an aberrant vascular loop of the anterior inferior cerebellar artery, the posterior inferior cerebellar artery or the intemal auditory artery.[19,29,30] A dilated, tortuous, atherosclerotic basilar artery may cause similar compression (as well as compressing additional cranial nerves simultaneously). Rarer causes include aneurysms and cerebellar-pontine angle tumours.[5,6,29] The most common proposed mechanism for the abnormal movements in this disorder is bidirectional ephaptic transmission and autoexcitation localized to the intracranial portion of the facial nerve.[31]
The postparalytic form may be caused by aberrant reinnervation of the facial musculature from branches of the functioning nerve that are proximal to the site of nerve injury. [6,11] Other theories include ephaptic transmission at the site of injury and spontaneous discharge from the deafferentated facial nerve.[6]
Differential Diagnosis
» Cranial dystonia
Several ocular and nonocular disorders must be considered in the evaluation of a patient with blepharospasm (Table I). [12,16,20-22,32-35] A thorough eye examination is indicated for external or internal eye problems such as dry eyes, inflammation, cataracts and retinal diseases that render the patient abnormally sensitive to light. One must search for foreign bodies on the external surfaces of the eyes, using magnification and lid eversion if needed.
Many neurologic disorders can cause lid spasms. Basal ganglia disease can produce various combinations of spontaneous blepharospasm, reflex blepharospasm and "apraxia" of eyelid opening, in addition to involuntary movements of the lower face. Patients with lesions of the upper brain stem or lower diencephalon usually have additional signs of brain-stem disease.
Blepharospasm is only rarely due to psychogenic factors. This diagnosis is quite difficult, especially in view of the response of organic blepharospasm to stress, its common association with depression and the unusual response of the movements to various stimuli.
The disorder probably most commonly confused with cranial dystonia is tardive dyskinesia. The classic form of tardive dyskinesia, caused by long-term treatment with neuroleptic drugs (dopamine receptor blockers), usually spares the eyelids. The buccal-lingual-masticatory area is most frequently involved. The movements associated with this disorder differ from those of cranial dystonia in that they are more typically choreic in their speed and flow and are often quite stereotypic. However, neuroleptics can also cause a chronic form of dyskinesia that mimics cranial dystonia ("tardive cranial dystonia").[3,16]
» Hemifacial spasm
The typical and postparalytic forms of hemifacial spasm are differentiated by the history of facial nerve palsy or injury. In the typical form the possibility of a posterior fossa neoplasm, although rare, must be ruled out by appropriate imaging studies.[5,6,19] Any additional cranial nerve dysfunction (e.g., in hearing or facial sensation) should prompt a detailed search for a definable cause.
Other disorders that can give rise to unilateral facial spasms include facial myokymia, tic disorders, focal seizures, demyelinating disorders, tetanus and, rarely, hysterical conversion reaction.[5,6]
Table 1 - Disorders considered in the differential diagnosis of blepharospasm
- Occiliar diseases
- External: foreign bodies, inflammation (of eyelids, cornea, conjunctiva)
- Internal: uveitis, cataract, retinal diseases
- Neurologic diseases
- Basal ganglia
- Common disorders: Parkinson's disease, postencephalitic Parkinson's disease
- Uncommon disorders: - Huntington's disease, Hallervorden-Spatz disease, acquired hepatolenticular degeneration
- Brain-stem and diencephalic disease: ischemia, demyelination
- Gilles de la Tourette's syndrome, other tic disorders
- Miscellaneous rare associations: seizure disorders, myotonia, tetany, tetanus, Schwartz-Jampel syndrome, progressive external ophthalmoplegia
- Pharmacologic side effects:
- Neuroleptics (tardive dyskiniesia, acute or tardive dystonia)
- Dopamine agonists (e.g., levodopa)
- Nasal decongestants (with long-term use)
- Inherited reflex blepharospasm
- Psychogenic disorder (hysterical spasms)
Treatment
» Cranial dystonia
If a patient with cranial dystonia is not disabled in any way by the abnormal movements, specific treatment may be unnecessary. Dry eye symptoms can be treated symptomatically with artificial tear preparations. When social or physical disability makes treatment necessary, both medical and surgical forms are available. In addition, some success has been obtained with biofeedback techniques.[36,37]
• Medical:
Where available, botulinum toxin injections have probably superseded oral medications as the first-line medical treatment for patients with severe or disabling blepharospasm. We review the results of therapy with this drug in a separate section.
Oral medications control symptoms on a long term basis in only 25% of patients with cranial dystonia.[3,38] In general, anticholinergics are used initially. Therapy with trihexyphenidyl hydrochloride is started at low dosages, 1 to 2 mg three times daily, and the dosage is increased by 2 mg every 1 or 2 weeks until the patient has a good clinical response or intolerable side effects.[3,39] Adverse effects include central nervous system disturbances such as memory loss, confusion, hallucinations and an unpleasant "high" sensation.[40] These complications necessitate a reduction in drug dosage. Peripheral side effects such as blurred vision, dry mouth, constipation and difficulty voiding may be reduced by the concomitant use of pilocarpine hydrochloride eye drops, a peripheral cholinergic agonist (e.g., ambenonium chloride) or both.
Initially favourable responses with dopamine agonists, such as lisuride, have been tempered by further experience.[41] Presynaptic monoamine-depleting agents such as tetrabenazine and reserpine can relieve symptoms in patients whose condition is refractory to other medications, although these agents frequently cause depression and parkinsonism.[3] Dopamine receptor blocking agents such as haloperidol, pimozide and phenothiazines can reduce the severity of dystonia in selected patients, although such patients risk the development of drug-induced parkinsonism and, more important, tardive dyskinesia.
Baclofen, clonazepam, lithium, lorazepam and cholinergic drugs such as choline and deanol acetamidobenzoate have been found to be effective in small groups of patients.[3,42]
• Surgical:
Patients whose blepharospasm component of cranial dystonia is not controlled with botulinum toxin injections or oral medication may be candidates for surgery. There are three surgical approaches available.
One approach is the avulsion of facial nerve fibres.[43-45] Up to 50% of patients treated with this technique require more than one operation to control the spasms, and even then in 50% of cases spasms recur 2 or more years after surgery. Gillum and Anderson[46] and McCord, Shore and Putnam[47] described a more effective procedure involving stripping the orbicularis oculi under direct exposure. It requires meticulous dissection while the patient is under general anesthesia. The frequency of reoperation has been under 25%.[46-48] Up to 75% of patients obtain significant subjective and objective relief for at least 12 months. A third approach is percutaneous thermolysis of the facial nerve branches to the orbicularis oculi.[49]
Pharyngeal dystonia affecting swallowing may be relieved by cricopharyngeal myotomy. Severe adductor-type spasmodic dysphonia may be alleviated by resection of one recurrent laryngeal nerve to improve phonation.[50]
» Hemifacial spasm
• Medical:
Some patients respond to carbamazepine,[51] but in our experience the response rate has been poor and benefit tends to be transient. Baclofen and clonazepam have been found to be useful in small numbers of patients.[51] Oral medications have generally proven much less effective than botulinum toxin injections or direct surgical decompression in controlling the spasms in both typical and postparalytic disease.[5,29,52]
• Surgical:
Success rates of over 90% have been reported with decompression of the facial nerve in the posterior fossa to relieve symptoms.[19,29,30,53] Postoperative spasm is frequent but subsides in most cases. Approximately 4% of patients require reoperation because of inadequate decompression.
Other options, such as crushing the facial nerve at its exit from the stylomastoid foramen, percutaneous fractional thermolysis, alcohol injections and anastomosis of the facial nerve with the 11th or 12th cranial nerve, usually provide only temporary relief and have not proven effective in most cases.[5]
Botulinum toxin injections
The use of botulinum toxin in treating eye disorders was pioneered by Scott,[54] who reported its use in correcting strabismus. Injections of small doses of botulinum A exotoxin into eye muscles were effective in altering eye misalignment yet were free of systemic side effects. After botulinum toxin was introduced in 1978 for the treatment of strabismus it was also found to be beneficial in the treatment of blepharospasm[55-57] and hemifacial spasm.[52,56,57] Tsui and associates[58] have successfully used the drug to reduce spasms in several patients with spasmodic torticollis. Botulinum toxin has also been effective in the treatment of spastic entropion (inturning eyelid).[59]
Pharmacologic features
Botulinum toxin is produced by the bacterium Clostridium botulinum. Eight antigenically distinct toxins are known, labelled A, B, Cl, C2, D, E, F and G.[60] Type A exotoxin has been used in the studies of eye disorders because this bacterial strain retains its toxigenicity well, and the type A toxin can be crystallized in a stable form.[54] The toxin acts on individual motor-neuron terminals. Its effects occur within hours of binding to the nerve cell membrane. The onset of action is gradual and continues until the end-plate potential is reduced to an extremely low level. The effect can last for several days or weeks.[54,60,61]
Although the precise mechanism of action is unknown, botulinum toxin probably interrupts calcium-mediated exocytosis of acetylcholine-containing vesicles at the axon terminal.[60,61] It does not block propagation of the nerve impulse and does not impair electrical excitability or conductivity in either muscle or nerve. Long-term exposure to the toxin causes denervation atrophy of muscle.[60,62]
The drug used in the treatment of ocular disorders is a lyophilized preparation of the neurotoxin. The drug is provided in vacuum-sealed vials, each containing 125 or 250 units of toxin activity. One unit is defined as the amount of toxin required to kill 50% of a group of 18- to 20-g female Swiss-Webster mice, and it is equivalent to 0.4 ng (0.0004 ,ug) of dried toxin.[55] On the basis of studies in monkeys[54] the median lethal dose (LD50) 70-kg human is approximately 2.0 µg. Patients treated for blepharospasm, dystonia or hemifacial spasm receive no more than 150 units (0.06 µg) of toxin per treatment.
Method of treatment
To treat eyelid spasms one injects the preseptal and pretarsal orbicularis oculi muscles in selected sites on each side with a 25- or 27-gauge needle attached to a tuberculin syringe (Fig. 1). For an initial treatment 0.1 ml (5 units) of botulinum A exotoxin is injected at each site.[55] If the eyebrows are in spasm the procerus and corrugator muscles are also injected.
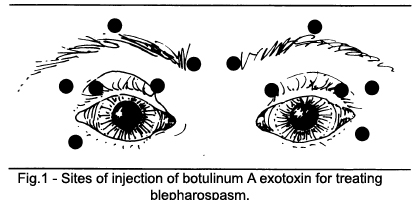 Figure 1 – Injection Points
Figure 1 – Injection Points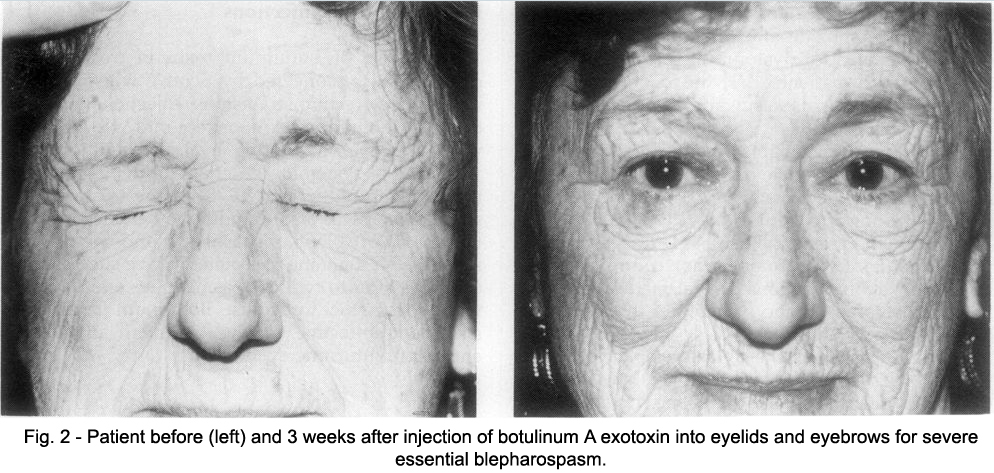 Figure 2 – Blepharospasm Patient Before and After Treatment
Figure 2 – Blepharospasm Patient Before and After TreatmentIn patients with hemifacial spasm the periocular muscles on the involved side are injected. In addition they receive injections to the lower facial muscles, as do patients with cranial dystonia who have spasms of these muscles. Thus, the perioral,paranasal, chin and cheek muscles can be weakened at the same time as the periocular muscles. Each of these sites is injected initially with 5 units.[52,55,56]
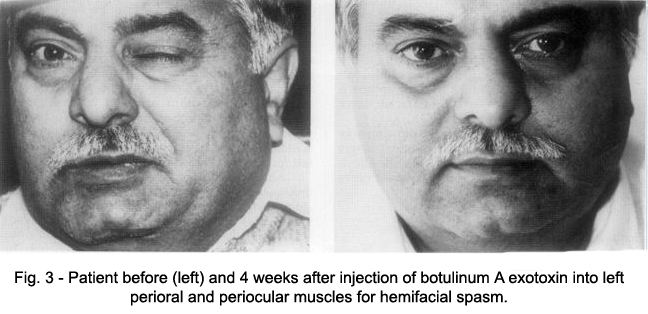 Figure 3 – HFS Patient Before and After Treatment
Figure 3 – HFS Patient Before and After TreatmentPatients with spastic entropion or benign eyelid fasciculations receive one or two injections (5 to 10 units in total) into the orbicularis muscle that is in spasm.[61] Spasmodic torticollis is treated with total doses the same as or greater than those for blepharospasm; the injections are made into neck muscles.[58]
Results of treatment
Complete or almost complete relief of symptoms is achieved in 85% to 90% of series of injections for blepharospasm (Fig. 2) and in 90% to 100% of series for hemifacial spasm (Fig. 3).[52,54-58] These represent substantially better results than those reported with oral medication for either condition. However, relief is temporary in almost all cases, lasting on average 3 to 4 months. Thus, injections have to be repeated periodically for an indefinite period.
As of June 1987 we had given 76 patients with blepharospasm 240 series of injections. In 209 series (87%) there was complete relief of eyelid spasms, for an average of 14.1 weeks. We had also given 20 patients with hemifacial spasm 44 series of injections; all series relieved the spasms, for a mean of 17.4 weeks.
The doses used in treating blepharospasm and hemifacial spasm do not stimulate a detectable antigenic response to circulating toxin.[63] In addition, double-blind studies in small groups of patients with bilateral blepharospasm have consistently shown objective improvement on the side of the face treated with the drug.[55,64]
Treatment with botulinum toxin has several advantages over oral and surgical therapies that result in a high rate of patient acceptance. It takes only approximately 15 minutes to perform. It is done on an outpatient basis, with no need for a local or general anesthetic. All reported side effects in patients with blepharospasm or hemifacial spasm were local ocular problems, including ptosis, dry eyes and tearing, due to excess eyelid laxity and were temporary in almost all cases.[52,55-59,65] In our patients the most common complications were ptosis (in 23% of treatments), dry eyes (in 18%) and tearing (in 5%).
The use of botulinum toxin in the treatment of several other forms of dystonia, including torticollis, spasmodic dysphonia and writer's cramp, is being investigated.[66-68]
– Article originally printed in the CMAJ, VOL. 139, NOVEMBER 1, 1988.
